Precision medicine, also known as personalized medicine, is an innovative approach to medical treatment and healthcare that takes into account individual differences in patients’ genes, environments, and lifestyles. The goal of precision medicine is to tailor medical care and treatment plans to the specific characteristics of each patient, with the aim of achieving the best possible outcomes.
Table of Contents
Introduction
The majority of medical therapies are one-size-fits-all and created with the “average patient” in mind. While some patients may benefit from them, others may not. Precision medicine—also referred to as “personalized medicine”—is a cutting-edge strategy that adjusts illness prevention and treatment based on individual variations in genetics, environment, and lifestyle. Providing the appropriate medications to the right patients at the right time is the aim of personalized medicine.
Precision medicine has already produced ground-breaking new findings and FDA-approved therapies that are customized to a patient’s unique traits, such as their genetic composition or the genetic profile of their tumor. Molecular testing is a standard element of patient care for patients with a range of malignancies, allowing doctors to choose treatments that maximize survival and minimize side-effect exposure.
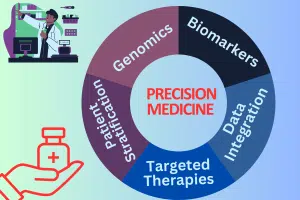
Key components of precision medicine
Genomics:
Analyzing the genetic makeup of an individual, including the study of genes, variations, and mutations. This information can help identify genetic factors that may influence a person’s susceptibility to certain diseases or their response to particular treatments.
Biomarkers:
These are measurable indicators, such as proteins or genetic mutations, that can be used to diagnose and monitor diseases. Biomarkers play a crucial role in identifying appropriate treatments for specific individuals.
Data Integration:
Precision medicine often involves the integration of various data sources, including genetic data, clinical data, lifestyle information, and environmental factors. Advanced technologies and computational methods are employed to analyze and interpret this diverse data.
Targeted Therapies:
Instead of using a one-size-fits-all approach, precision medicine aims to develop targeted therapies that are specific to the characteristics of individual patients. This may result in less harmful treatments that are also more effective.
Patient Stratification:
Personalized medicine allows for the classification of patients into subgroups based on their unique characteristics. This enables healthcare providers to better understand disease heterogeneity and tailor treatments accordingly.
It has made significant strides in various fields, including oncology. For example, certain cancer treatments are now designed to target specific genetic mutations present in a patient’s tumor, increasing the likelihood of treatment success. The use of precision medicine is expanding to other areas of medicine, offering the potential for more accurate diagnoses, individualized treatment plans, and improved patient outcomes.
Read Also: 100 Questions and Answers About Pharmaceutical
The activities of pharmacists in precision medicines
Pharmacists play an essential role in the implementation and management of precision medicine, also known as personalized medicine. Precision medicine is an innovative approach to medical treatment that takes into account individual differences in patients’ genes, environments, and lifestyles. The goal is to tailor medical care to the characteristics of each patient, allowing for more targeted and effective treatments.
Here are some key aspects of the role of pharmacists in precision medicine:
Genomic Testing and Interpretation
Advising Patients:
Pharmacists may help educate patients about the benefits and risks of genomic testing, as well as assist in obtaining informed consent.
Interpreting Results:
Pharmacists with expertise in genomics can interpret genetic test results and provide relevant information to healthcare providers and patients.
Medication Selection and Dosing
Tailoring Treatments:
Pharmacists can use genetic information to help healthcare providers select medications that are most likely to be effective for a particular patient.
Dosing Adjustments:
Based on genetic variations, pharmacists can recommend personalized dosage adjustments to optimize drug efficacy and minimize adverse effects.
Drug-Drug Interactions
Identifying Risks:
Pharmacists are trained to identify potential drug-drug interactions, and in the context of precision medicine, they consider genetic factors that may affect how a patient metabolizes drugs.
Providing Recommendations:
Pharmacists can recommend alternative medications or dosage adjustments to minimize the risk of adverse reactions.
Patient Counseling
Education:
Pharmacists play a key role in educating patients about precision medicine, including the importance of genetic testing and how it influences treatment decisions.
Adherence Support:
They can provide guidance on medication adherence, potential side effects, and the importance of regular follow-up appointments.
Collaboration with the Healthcare Team
Communication:
Pharmacists collaborate with other healthcare professionals, including physicians and genetic counselors, to ensure a comprehensive and coordinated approach to precision medicine.
Monitoring:
They participate in monitoring patients for treatment response and adverse effects, adjusting therapies as needed.
Continuing Education
Staying Informed:
It is a rapidly evolving field. Pharmacists need to stay informed about the latest advancements, guidelines, and research to provide the best possible care.
In summary, pharmacists are essential members of the healthcare team in the era of precision medicine. Their expertise in medications, drug interactions, and patient education positions them to contribute significantly to the safe and effective implementation of personalized treatment plans for individuals based on their unique genetic makeup.
Read also: What is Pharmacovigilance?
The activities of pharmacies
Pharmacies play a crucial role in the implementation and dissemination of precision medicine, which is an innovative approach to healthcare that considers individual variability in genes, environment, and lifestyle.
Here are several ways in which pharmacies contribute to the success of precision medicine:
Dispensing Personalized Medications
- It often involves tailoring medications to the specific genetic makeup of an individual or a subgroup of patients.
- Pharmacies are responsible for dispensing these personalized medications based on genetic information and other relevant factors.
Genetic Testing Services
- Some pharmacies may offer genetic testing services to help individuals understand their genetic predispositions and responses to certain medications.
- The results of these tests can guide healthcare providers in prescribing medications that are most likely to be effective and have minimal side effects for a particular patient.
Patient Education
- Pharmacists play a key role in educating patients about precision medicine, including the importance of genetic testing and how it can impact medication selection.
- They can help patients understand the implications of their genetic information and empower them to make informed decisions about their treatment plans.
Adherence Monitoring
It often involves complex medication regimens. Pharmacists can help monitor and promote patient adherence to these regimens, ensuring that patients follow their prescribed treatments as closely as possible.
Collaboration with Healthcare Providers
Pharmacies collaborate with healthcare providers to implement precision medicine strategies effectively. This collaboration may involve sharing information about patients’ genetic profiles and medication responses.
Data Management
It relies heavily on data, including genetic information and patient outcomes. Pharmacies may play a role in managing and safeguarding this data, ensuring privacy and adherence to ethical standards.
Clinical Decision Support Systems
Pharmacies may integrate clinical decision support systems that help healthcare providers make informed decisions about medication selection based on individual patient characteristics, including genetic information.
Medication Therapy Management (MTM)
Pharmacies can provide MTM services to optimize medication use. This includes reviewing patients’ genetic profiles to identify potential drug interactions, adverse reactions, or the need for dose adjustments.
Access to Specialized Medications
Some precision medicines are novel and may not be readily available at all pharmacies. Specialty pharmacies, often affiliated with larger healthcare systems, may be involved in ensuring the availability and proper distribution of these medications.
Conclusion
In summary, pharmacies are integral to the successful implementation of precision medicine by facilitating the dispensing of personalized medications, offering genetic testing services, educating patients, collaborating with healthcare providers, managing data, and ensuring adherence to treatment plans. Their role extends beyond traditional medication dispensing to actively support the individualized and targeted nature of precision medicine.
Frequently Asked Questions (FAQs)
What is precision medicine?
Precision medicine, also known as personalized medicine, is an innovative approach to medical treatment that takes into account individual differences in patients’ genes, environments, and lifestyles. By tailoring medical care to the specific characteristics of each patient, precision medicine aims to improve treatment outcomes and minimize adverse effects.
How does precision medicine differ from traditional medicine?
Unlike traditional one-size-fits-all approaches, precision medicine considers the unique genetic makeup and other individual factors that contribute to a person’s health. Traditional medicine often relies on generalized treatments for a particular condition, while precision medicine seeks to customize treatments based on the specific characteristics of each patient.
What role does genomics play in precision medicine?
Genomics, the study of an individual’s complete set of genes (genome), is a key component of precision medicine. By analyzing a patient’s genetic information, healthcare professionals can identify genetic variations that may influence disease susceptibility, treatment response, and potential side effects. This information helps in tailoring treatment plans to each patient’s unique genetic profile.
Which diseases can benefit from precision medicine?
It has shown promising results in various medical fields, including oncology, cardiology, and rare genetic disorders. It is particularly impactful in the treatment of cancers, where genetic profiling of tumors can guide the selection of targeted therapies. Additionally, precision medicine is increasingly being explored for conditions such as cardiovascular diseases, neurodegenerative disorders, and autoimmune diseases.
What are the difficulties associated with implementing precision medicine?
Despite its potential benefits, precision medicine faces challenges such as cost, data privacy concerns, and the need for widespread genetic testing infrastructure. Additionally, interpreting complex genetic data and integrating it into clinical decision-making can be challenging. The ethical implications of using genetic information in healthcare and addressing disparities in access to precision medicine are also important considerations in its implementation.

Abdus Sobhan Salim is professional experienced pharmacist in pharmaceuticals, author and founder of pharmabossbd.com, the first Bangladeshi pharmaceutical blogger since 2019.